Love, Unbroken
I emailed Bren’s treating hospital last Wednesday. I’m impatient, I couldn’t wait any longer to find out what was happening with his treatment plan. I know being impatient doesn’t make things move any faster, but at least I felt better after sending the email. On the other hand, Bren was still being impressively patient; he is a saint. I am not.
July 20, 2014
Finally, it’s all go! We will find out the treatment plan details this Tuesday, and are packing for the city, ready to get his recovery underway. We’re hopeful. Bren has no idea how he will tolerate chemotherapy, but he will do whatever it takes to rid himself of cancer. He has two kids to raise.
Sometimes, I scream uncontrollably on the inside at the thought of my husband going through all this. I was recently told that when having Chemo, you realise how sick you have to be before you’re dead. It was a shitty thing to hear. The person who said it didn’t mean to scare me; she had chemotherapy herself and was telling a simple truth. It’s horrendous, and we are stronger than we think. Human beings can fight and win against incredible odds. I asked Bren how he was doing as we made our way to the car. He said, “I have two choices. I can fall in a heap or keep moving forward.” He has never been one to stand still or take a backward step. He will always choose to move forward.
July 22, 2014
Today we met the oncology team—Dr. V and Taya, his temporary Clinical Nurse Consultant (CNC). Tomorrow, Bren will begin his first of several chemotherapy infusions, aimed at shrinking the tumour as much as possible before surgery.
Taya, who is covering for Krista (the regular CNC we’ll meet next time), is warm and a very fast walker. She is in her late 20s or early 30s. She’s tall, with a shoulder-length brown bob, and always seems to be in motion, often darting off to handle other tasks. Despite her busy schedule, she’s approachable and efficient. She’ll be working closely with Sandra, Dr. Brach’s CNC, to coordinate Bren’s appointments and help maintain open communication between us and the medical team.
Bren’s first appointment today is to have blood taken, and then we wait. About 45 minutes to an hour later, Taya finds us and walks us over to Princeton Imaging for a CT scan. We find out after the scans that Bren shouldn’t be walking anywhere without a pair of crutches, using the one he got after his biopsy isn’t enough support, because of the crack in his femur from the tumour. He isn’t supposed to be driving, either. And he is not happy about that! More waiting follows, and then we head upstairs to meet Dr. V, Bren’s oncologist. This consultation takes about an hour. Dr. V is around Bren’s age; he is tall and fit. He has great skin, no hair, and is in no rush to get us in and out. He is calm, speaks slowly, and talks to us in easy-to-understand terms.
It’s easy to see why Taya is impressed by Dr. V and grateful for the opportunity to work with and learn from him, and it’s good to know Bren has the right oncologist. She tells me that he specialises in paediatric cases, and we are fortunate to have him on Bren’s team.
At this consultation, we hear what type of cancer Bren has for the first time. We knew it was a sarcoma, but now it has a name: Undifferentiated Pleomorphic Sarcoma. John Green was right, I think; it seems the more syllables there are, the more dangerous it is. I am sure he said something like that in A Fault in Our Stars. Anyway, it seems to be true. Bren’s is a rare and aggressive type of cancer. We listen carefully to the information Dr. V is sharing. I blink hard when I hear the worst-case scenario is death. I don’t want to cry. It’s hard not to. Hearing Bren could die shocks us both. Logically, we knew that. Everyone knows cancer can kill. But not my husband. I wasn’t ready to hear it could kill Bren. Then, for the second time since being diagnosed, we hear this type of cancer is highly treatable. I’m relieved to the point of feeling faint. So, this is what I heard: ‘ What you have, Brendan, is exceedingly rare. It is more common in children and teens than adults. And it is highly treatable.’ I could kiss Bren and the doctor. It is highly treatable. After the oncology consult, we have another long wait before Bren’s next appointment. It will be ‘education’ with Ken, the nursing practitioner at Day Therapy, regarding Bren’s chemotherapy tomorrow
Ken is fabulous, kind, gentle, and generous with his time. He has six phones on the go, and everyone wants a piece of him. He is there for staff, patients, and carers. He seems to thrive on chaos. Ken explains the process and protocol of Bren’s treatment to prepare him for tomorrow. There is a lot of information to take in, and then he goes through all the possible side effects. I glance at Bren. I cannot tell how he’s feeling, but I’m nervous.
It has been a long day. Sitting in our favourite cafe on Prince Street, conveniently situated nearby, we sip cappuccino and debrief our day. A white paper store bag with black branding sits on the empty chair at our table; inside are two kids’ T-shirts. I make a mental note not to leave it behind when we leave.
“You, OK?” I asked
“I’ll tell you tomorrow,” Bren smiles as I squeeze his hand.
“Big day, hey!”
“Yep.”
We finish our cuppas, I grab our purchase, and we head back to our accommodation to rest.
July 23, 2014
We are both pale and bleary-eyed when we turn up at Day Therapy. We are the first ones there. The reception area is a bright, airy room with a coffee and tea bar opposite the reception desk. The furniture is modern, in caramel, cream and coffee colours, and has two widescreen TVs. The Morning Show is on. We sit for almost an hour before being called into Bren’s cubicle by Regan, or Reg as she was better known. She is the treating nurse on Bren’s team of three today, who will all be checking in on him throughout the next 8 or 9 hours. She is pretty, very tall, with beautiful straight red hair, freckles and rosy cheeks. Reg goes over education again, even though Ken had gone through it with us the day before. There is a fair bit of repetitiveness. We are new to the cancer rollercoaster. The team needs to be sure we understand what is about to happen. Reg then explains the remotes for Bren’s chair. One is for him and the other for staff.
“Don’t mix them up.” she teased, explaining that the staff’s remote button is for emergency incline.
She smiles at Bren and says, “You won’t need that.”
Bren will receive two Chemo drugs today. A magnesium infusion will follow. One bag will take 20 minutes, and the other, plus the magnesium, will take around 7 hours. The side effects of each drug are explained when administered. The 20-minute drug, if not given correctly, has horrific side effects. The cannula needs to be inserted into Bren’s vein precisely, there is no room for error. Reg assures Bren that they check for blood return three times before the infusion goes ahead to ensure the cannula is in the right place. As a part of education, Reg also explains that if the needle goes into the flesh and not the vein, the drug will eat his flesh. If this happens, Plastics will be called to treat the area immediately. In the worst-case scenario, it could result in amputation. Shit! I hate the worst-case scenario; it’s always horrific! OK, the cannula is in; first check, no blood return, shit! Second check: no blood return! Another team member consults, and he checks. No blood return! Ken consults, gets a phone call, takes it—excuses himself, comes back, checks again—no blood return! Shit! He double-checks the line has a good flow; the infusion can start. Shit!! Double Shit! Bren squeezes my hand hard. The first lot of ‘get him well’ poison enters his body; it’s an anxious 20 minutes as this infusion progresses. We all sigh with relief when it finishes.
“OK, you get to keep your arm this time!” Reg says, smiling cheekily. “We’re all very good at this Brendan; none of us wants the worst-case scenario on our conscience or our record.” she gives him a, we’re in this together wink, sets up the next infusion and moves on to her next patient.
I’m glad the first step is over. Now we have time to kill. We chat and get to know the team better as they come and go. The volunteers bring iPads to pass the time and fresh sandwiches, muffins, biscuits, juice, coffee, and tea to Bren’s cubical for both of us. We are feeling well cared for. Carey comes in and pulls up a chair; he is the nurse in charge at the front desk. He’s lovely. Carey’s dad lives at Harrington, 5 to 10 minutes from where I grew up. It’s a small world. I like him. Carey has a lovely face, kind eyes, a gentle manner and is here to help in any way he can. He asks how we are feeling and what we might need. He chats about our kids and family and reminds us that this situation is tough on everyone. Psychologists and counsellors are available through the clinic for anyone who needs them. After handing me some pamphlets, Carey looks square at me and asks how I am. I tell him I’m OK.
“This is hard on you because everything will fall on you! You will be taking on double the load. When Brendan sleeps through the day, you sleep, too; you must take care of yourself!” He councils compassionately. We chat for a bit longer, and then he returns to the front desk.
Bren is starting to fade in and out while receiving his magnesium infusion as the other drugs take effect. He looks pale. He asks if I can give him some Reiki. I stand behind his chair, place my hands on his forehead, and feel the energy start to flow. I notice he’s sweating. He tells me he wants to throw up. I stop what I’m doing to grab a vomit bag and press the nurse’s bell. Too impatient to wait, I get Carey from the front desk. He takes one look at Bren and calls Reg. I sense anxiousness; they are both on their phones, and Reg hits the big red emergency button on the wall beside Bren’s chair. Carey gently takes me by the arm and whispers, “Come with me, sweetie,” as he guides me out of the cubical.
It feels like an out-of-body experience as I watch everyone move around quickly in slow motion. The small room fills with nurses, and they spill into the hall. Someone calls for the ‘cart.’ Shit! I feel my heart stop. Reg pushes the emergency incline button. And all I can see are my husband’s feet.
Breathe, breathe, I tell myself as tears roll down my cheeks. Carey is standing beside me, writing down numbers being called out by a different nurse; he mouths to me, “He’s OK. He’s OK.”
The Sister in charge of the ward and Ken are in the room now. Along with the prettiest registrar I’ve ever seen. She looks like she has stepped straight off a catwalk to be here. Tall and willowy with long sandy blond hair pulled back in a pony, she wears a pencil skirt, striped collared shirt, and a black sweater. I thought, crap, Bren might look up and think he’s gone to heaven. She’ll scare the bejesus out of him.
The sister came over to the cart near where I was standing. She grabbed the defib paddles from their case, and I thought I would pass out. It’s clear I’ve watched too much ER over the years. She disconnected them from their leads and attached the leads to Bren to get a clear trace from his heart. OK, that’s alright! I saw him crane his neck to find me, and he gave me the thumbs up. Then I heard him laughing, and I knew he was OK. He recovered fast, and when all his readings were back to normal, the sister told him she wished she had an ECG like his.
“What did you think when you saw that beautiful registrar?” I asked him.
“Aww, she was alright, but when you have people looking after you like that, they all look pretty good,” he said, smiling.
This ordeal unfolded in just a matter of minutes. The response was phenomenal. And the rest of the treatment went without a hitch. However, there were many jokes that afternoon about our drama queen, helping to lighten the mood for the rest of the day’s treatment. We know now that Bren reacted to the magnesium. The team will change the prescription before his next treatment.
August 2, 2014
Standing in the shower, I let the hot jets of steaming water wash over me. I could hear Bren playing his guitar from where he sat at the foot of our bed. It was one of his favourite ways to pass the time.
“What’s that you’re playing?” I yelled. No answer.
I turned off the taps, squeezed the water from my hair, grabbed a towel and stuck my head out the ensuite door.
“What are you playing?” I said again, “It sounds nice.”
“Just something I’ve been working on.”
“Babe—it’s great. Did you make it up? I love it.”
“Lucky, it’s your song.”
“Mine,” I said as tingles floated across the top of my arms.
“What’s it called?”
“Your song.” He looked up from the strings as he played, grinning at me.
I pulled on my PJs and sat beside him to listen some more.
“Oh my God, I love it,” I said, kissing him as he turned his face toward me.
“Good!” He replied, bumping me gently with his shoulder as he played.
“Babe, there’s lots of hair on the shower floor,” I said, watching his fingers move effortlessly across the chords.
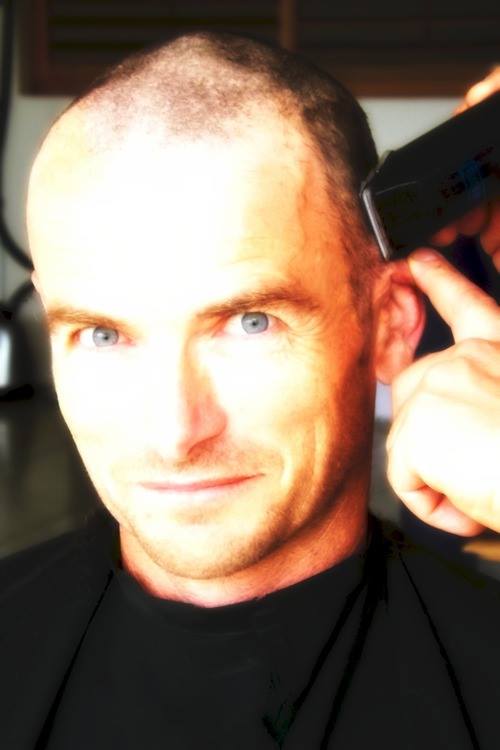
“Yep!” He said, letting out a breath he’d held onto a few seconds too long. “I’ll ring Dean to come and shave it off. He’s wanted to take to me with hair clippers for years. He said he’d come when I’m ready.”
“You sure you’re ready?”
“Yep. It doesn’t worry me that much, losing my hair. It just makes it more obvious I’ve got cancer.”
“Yeah, it’s shit, babe.”
“I don’t want people to feel sorry for me.”
“I don’t want that for you either. But babe, you’ve got cancer. People are going to feel sorry for you. It’s normal. Having a bald head will be the only obvious change. Lots of people are bald.”
“Yeah, but usually they’ve got eyebrows and eyelashes.” He said, screwing his nose up as he glanced back at me.
“You still look fit. You’re hot, babe.” I said, nudging him in the ribs with my elbow.
“People will react to you, not to cancer. I promise. Right! What do you want for dinner?” I said, getting up to go to the kitchen.
“Something that doesn’t taste like metal, please.”
“I’ll do my best,” I said in the least sympathetic tone I could muster. “But you know my cooking, no promises.”
Bren’s hair loss happened sooner than expected. His once-thick hair was gone; he was bald, and he was right. He looked every bit like a cancer patient because he was. At least he was feeling well.
August 7, 2014
In the city again, in prep for more Chemo, Bren had a blood test and CT scan before his clinic appointment to ensure chemotherapy could go ahead the next day. We went window shopping afterwards, while he felt well enough to get out and about, before returning to our accommodation and heading to a great local pub a block away for an early dinner. An early-ish night followed to prepare for the long day coming up, in day therapy. Chemo went without a hitch this time, and many staff who remembered Bren from his last treatment complimented his new clean shave. We were back at the motel, and Bren was in bed by 7:30 p.m. and was not well. There would be no dinner out tonight.
By 11 pm, right on cue, Bren’s reaction to the chemo hit—just as it had after the last infusion. Waves of nausea, relentless vomiting, and a crushing motion sickness left him collapsed on the floor of the cramped, caravan-sized bathroom. He couldn’t lift himself, and I wasn’t strong enough to lift him back to bed. All we managed to do was get him upright enough to reach the toilet bowl. The ordeal dragged on into the early hours of the morning, and all I could do was hold him. Watching him suffer was utterly soul-destroying.
The car seemed to sigh with relief as it rolled into our driveway the following afternoon, its engine heaving to a stop. I glanced at Bren, his eyes heavy with exhaustion, mirroring the weariness I felt settling into my bones after the long, miserable trip home. He said a quick hello to the kids, and Margaret and I got him into bed. The days that followed were terrible.
August 18, 2014
With this lot of chemo, Bren’s side effects have worsened, and eating has been especially problematic. Some nights, I lay beside him as he slept, listening to his laboured breathing, or sat close by watching him lay exhausted on the lounge and thought, how did this become our story? How did everything change so quickly?
In the leadup to his diagnosis, he had mistaken symptoms for a persistent, niggling sports injury. Would it have made a difference if we had caught the tumours earlier? Probably, but that’s something we’ll never know. There are so many questions with no answers. All we can do is keep going. Like last time, day eight post-chemo was Bren’s turn-a-corner day, and day 9—his, if I don’t find something to do, I’m going to go crazy day! Even so, he is quickly exhausted. An hour of doing anything means he’ll need to rest for a few hours afterwards. He doesn’t let that stop him. Bren’s next treatment is coming up quickly. An oncology review will follow.
September 4, 2014
Treatment Review
It’s spring, yet as the alarm wakes us with the sun, to head down to the city, it feels more like the middle of winter. I want to pull the covers around me and keep dreaming about the brown heels with the mesh centre strap I was about to buy from my sister Sue. This week has felt disorganised. I cannot see the floor in the kid’s playroom, and Bren and my bedroom is not much better. The whole house is a minefield. I had forgotten to book our accommodation; luckily, when we rang yesterday, they could squeeze us in. We didn’t allow for the fact that the Roosters and Rabbitohs had a big football game on. Their fans had all but booked out our stay of choice. I showered, warmed up, had breakfast, hugged the kids, thanked my sister, and we were out the door on time until I realised, I couldn’t find my driving glasses or the Navman. We found them in the “sick bucket” half an hour later. The bucket would typically have been coming with us, except that Bren does not have Chemo this time, so it was still in the cupboard, with glasses and Navman inside.
Off we go, neither of us very happy, but we’re on the road. Bren is still not feeling fabulous; he hasn’t bounced back as well from the Chemo this time. We get into the city by 11:30am; by the time we park and get to where we need to be for his MRI, we have 10 minutes to spare. An hour or so later, it’s back over to ROCC for the CT scan, and then another hour later, we’re right to go. No walk down to Parment Road or up to Prince Street today. We go straight back to our room, and Bren sleeps for the rest of the afternoon.
September 5, 2014
It was damp and miserable outside, as I ate breakfast alone. Bren was nil by mouth in prep for his PET Scan. Our motel was a popular truck stop, and two big, burly blokes were also having breakfast. The two truckies, the day manager, and I were a funny mix. We sat at different tables, with the manager behind his desk, sharing one conversation. I liked that; it was a good way to start the day.
I left Bren for his PET Scan when we got to Princeton and returned to the ROCC lounge to fill in the next couple of hours. After quickly checking messages on one of the computers in the family room, I lay down on the oversized beanbag to read for a bit before giving myself a reiki treatment. Just after noon, I met Bren and we went upstairs for the treatment review. There was good news and bad news. The good news was that the Chemo has done what it was supposed to and stopped all present tumours from growing or spreading. There was no evidence of any others forming. The bad news was Dr. Brach was sick, and the MRI and PET scan reports were not ready for the meeting. Dr. V, Krista, and Dr Brach’s CNC Sandra filled us in on what they could. At this stage, the tumour removal could be tentatively scheduled.
September 15, 2014
All going well; Bren will be in on a Monday, out on Friday and the tumour will be gone. Then, approximately two weeks later, he will have more Chemo, and finally, Dr. Chen will remove two tumours from Bren’s lungs. And that will be it. All done, no more Chemo, finished, bring on the party!
We left the clinic feeling weary, but quietly relieved. Still, we would have liked to speak with Dr. Brach, but even doctors get sick. We may need to make another trip to the city later this week to see him. The good news is that the results were what they needed to be for the operation to proceed. Now, all that remained was Dr. Brach’s final sign-off on the scheduled dates.
It had been a long, emotionally draining day. The lead-up to a clinic review are always tense. For Bren, it must feel like sitting before God, waiting to hear if he gets to live a little longer. But they are a necessary part of the process and will continue to be scheduled every 3 months, even after chemo is finished, until Bren is out of the woods.
By the time we got back to the car, it was 2:30 in the afternoon, with hours of driving ahead. But we were driving home knowing the surgery would go ahead. That was a win.












Leave a comment